"I was amazed at how quickly Cortigon leveled me out after I started taking it. It has helped me to maintain a sense of calm and balance through out the day, especially when things start to pile up. Cortigon will remain a regular part of my daily supplements."
Tim M.
Verified Buyer - Results may vary by individual.
CORTIGONNatural Stress Relief & Cognitive Support
$44.99
CORTIGON is all about supporting a healthy stress response, mood and focus, and healthy brain function.
CORTIGON supports you with a natural balancing of hormones, improved mental clarity, overall improved brain function, as well as increased energy & memory retention.†
Memory
Focus
Mood
Subscription
$44.99
Quantity
Free USA Shipping On Orders $75+
60-Day Money Back Guarantee
Featured Add-Ons:
CORTIGON is all about supporting a healthy stress response, mood and focus, and healthy brain function.
CORTIGON supports you with a natural balancing of hormones, improved mental clarity, overall improved brain function, as well as increased energy & memory retention.†
Memory
Focus
Mood
Subscription
$44.99
Quantity
Free USA Shipping On Orders $75+
60-Day Money Back Guarantee
"I was amazed at how quickly Cortigon leveled me out after I started taking it. It has helped me to maintain a sense of calm and balance through out the day, especially when things start to pile up. Cortigon will remain a regular part of my daily supplements."
Tim M.
Verified Buyer - Results may vary by individual.
CORTIGON is all about supporting a healthy stress response, mood and focus, and healthy brain function.
CORTIGON supports you with a natural balancing of hormones, improved mental clarity, overall improved brain function, as well as increased energy & memory retention.†
Memory
Focus
Mood
Experience a true sense of calm. Support mood, focus & stress management with CORTIGON.
Memory
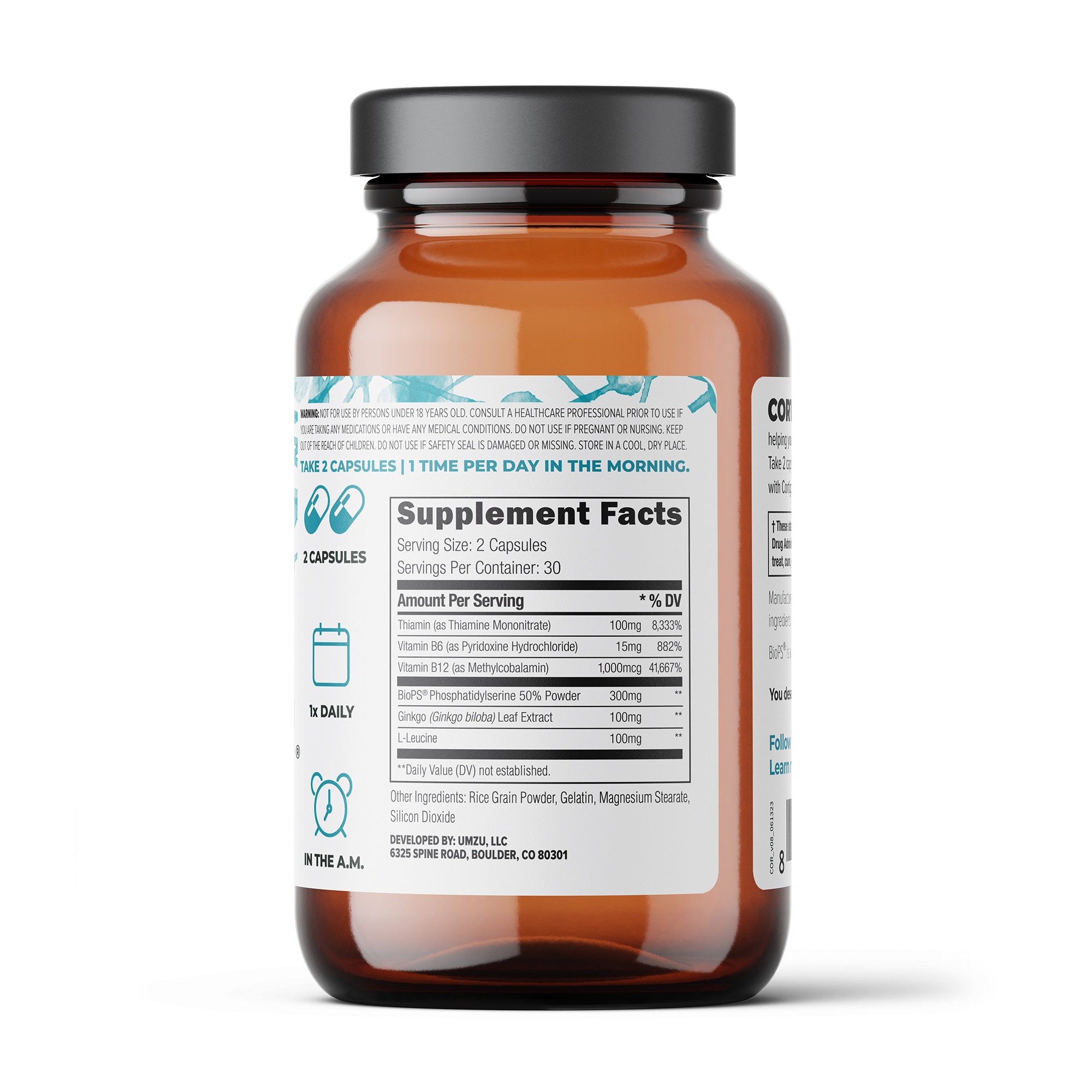
The cognition-supporting ingredients in CORTIGON, to include Phosphatidylserine, Ginkgo Biloba, Vitamin B12, & Vitamin B6, work synergistically together with the body to support healthy memory & brain function.†
Focus
Support mental clarity & focus with CORTIGON. The ingredients are formulated to nourish the brain’s neurotransmitters, support hormonal health & stress response, & support healthy neurological function.†
Mood
Negative stress, mood fluctuations, and varying energy levels can be overwhelming. Support a healthy stress response, a lift in mood, & healthy energy production with the help of CORTIGON.†
Support a stressful life. Naturally.
CORTIGON is expertly blended with key ingredients that naturally support the health of your brain - resulting in a healthy response to stress and improved stamina, focus and mood. CORTIGON by UMZU is a thoroughly research-backed blend of natural herbs, vitamins and minerals of the highest possibly quality, that are shown in research to help reduce production of the stress hormone cortisol. CORTIGON has been used by tens-of-thousands to support a healthy stress response, improve memory and experience a sense of calm.†
- 6 Natural Ingredients
- Stress Management
- Focus
- Memory
- Mood
- Research-Backed
Supplements don't need a long list of ingredients to be effective. In fact, the more ingredients in a supplement, the less likely it is to have the minimum effective levels of each ingredient.
CORTIGON is a simple yet incredibly effective 6-ingredient formula containing at or above the recommended effective dose for daily usage of each.
-
Option 1: Relieve daily stress by taking 2 CORTIGON capsules in the morning.
-
Option 2: Need to focus on important tasks? Take up to 4 CORTIGON capsules for a noticeable increase in focus and mental clarity.
-
Upgrade Your Brain: Pair CORTIGON with MUCUNA PRURIENS and MIRACLE MORNING for a cognition-boosting stack.
Nature does the work. Ingredients in CORTIGON:


P.S. (Phosphatidylserine), We Love You.
Natural products you can trust
No Harmful Fillers
Thermo-Approved
Natural Ingredients
cGMP Manufactured
Research-Backed
Assembled in the USA
Lab Tested
Any questions we haven't answered? We're here to help.
Frequently asked questions about CORTIGON and important things to consider when using the product.